Credit: Pixabay / CC0 Public Domain
Inherent in all people lies the ability to treat many of the most common diseases. Hidden compounds – or natural products – are waiting to be discovered, decoded and restored for this purpose.
Chemists such as Jason Crawford, associate professor of chemistry and associate professor of microbial pathogenesis, have been studying these natural products for years. These small molecules, known as specialized metabolites, are derived from our metabolism and are widely used as drugs or drugs to treat a variety of diseases. Evolutionarily designed for perfect structures over millions of years, they regulate a wide range of biological phenomena. The problem is that most of these molecules are not available to us because they remain unknown.
In his lab at the Yale Institute of Biomolecular Design and Discovery on the West Campus, Crawford and his research team of graduate students and postdocs hunt for genetically encoded molecules, or GEMs, in a sea of molecules in the human body (or host). GEMs are important because they can be converted into drugs to treat cancer, infectious diseases, inflammatory bowel disease (IBD), psoriasis and many autoimmune diseases.
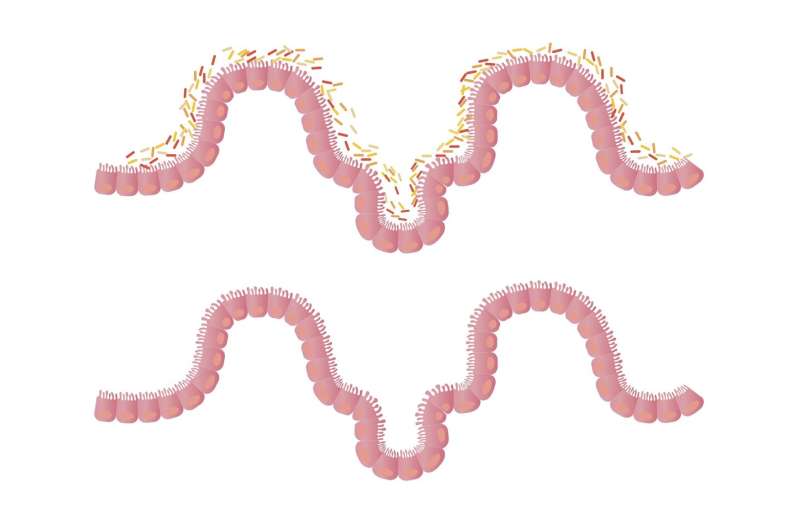
Crawford Lab studies metabolism at the host-microbe interface. Most of the microbes they look at are either known human bacterial pathogens or environmental isolates from IBD patients collected by his collaborators in the Yale Immunobiology department. This collection of disease-associated bacteria often produces unique GEMs that positively or negatively modulate the severity of the disease.
We recently spoke with Crawford about his research into natural molecules and their potential medicinal properties. This interview has been edited for clarity and space.
Can you share one of your latest discoveries?
What I am most excited about right now is our recent discovery of a new metabolic pathway in humans and mice in this cell type called the macrophage. It is an important innate immune cell type. Prior to our decoding efforts, mutations in that gene were associated with a wide range of inflammatory diseases, such as arthritis, IBD, and leprosy, a type of microbial infection. We also found that the gene facilitates the elimination of microbial infection, which means that if you have a dysfunctional copy, you are much more susceptible to infection.
When we decoded the road, we found that you could add the product of the road – the connection – back, treat animals and largely restore wild-type activity. What’s nice about it is where gene editing is still largely experimental and not yet available to human patients with genetic defects, however molecules are available to treat a wide range of inflammatory diseases.
You and a team of Yale researchers recently received a $ 8.5 million grant. from the National Institute of General Medical Sciences of the National Institutes of Health to explore the role of microbial metabolites in the human gut. Congratulations! Tell us more about this initiative.
In this project, we try to identify small molecules that regulate ‘orphaned’ G-protein-coupled receptors (GPCRs). GPCRs are the most medicated receptor family in the pharmaceutical industry.
We call a subset of these ‘orphans’, which means we do not know which molecules control these receptors. These receptors often determine new biological phenomena. The molecules that control them can tell us about the chemical signaling processes that we do not yet know. This grant focuses in particular on orphan GPCRs and our efforts to decode the molecules that regulate them.
The goal is, let’s say, five years later, that we have identified three different sets of molecules that regulate three different orphaned GPCRs. It could open up three entirely new areas of chemical signaling in humans. These can also be medicinal targets based on the history of medication of GPCRs for the biological processes.
So the grant itself is an academic endeavor to decode the unknown. The pharmaceutical relevance downstream would be to medicate these new biological processes for the treatment of diseases.
Can you talk about how the microbiota – the bacteria in our gut – interact with our immune system and your work in that space?
We are investigating compounds as therapeutic agents for inflammatory diseases in collaboration with Richard Flavell (Immunobiology). We have at least five collaborations with Richard’s laboratory in the field of metabolism analysis at the molecular level to identify how microbiome members regulate unexplored areas with inflammatory signaling.
What is important to know about these efforts is that microbes use a wide range of molecular mechanisms to regulate inflammatory processes, and we know of only some of them. So if we screen the microbiome for small molecules that regulate non-canonical signaling results, then we can detect the responsible molecules and reuse them as ‘molecular probes’ to try to separate the signaling pathway from each other. These efforts can allow us to discover new areas of inflammation. Once we detect them, dysregulation of the same processes may underlie various inflammatory diseases. We must first understand them before we can figure out how to treat them. Connecting microbes to these processes tells us which microbiome members either aggravate or alleviate the associated inflammatory diseases.
One of the inflammatory programs that we study is extra-intestinal inflammatory immunopathologies, which are associated with Crohn’s disease. Crohn’s disease is one of the inflammatory bowel diseases, but a subset of these patients have extra-intestinal inflammatory conditions, and the microbiome also mediates them.
We question how the microbiome can regulate inflammation far away from the gut. One way is to produce molecules, and then those molecules gain access to what we call ‘systemic circulation.’ many of these projects are collaborative.
What other ways is the Crawford Laboratory focused on inflammation?
We still have a study with Noah Palm (immunobiology) and Seth Herzon (chemistry), where we have decoded additional genotoxic pathways from the intestinal microbiome.
With our previous coursework, Seth and I decoded a pathway associated with the initiation of colorectal cancer. We have recently decoded additional pathways from microbiome members that cause tumor formation. Some might think that our previous work with colibactin was a single time, but we have now decoded several pathways associated with cancer. Noah discovered bacteria that regulate tumor formation in mice, while our contribution was to find out which molecules are responsible for regulation.
So how does this circle go back to inflammation? The genotoxicity of microbes causes cellular damage, and cellular damage is another way to regulate inflammation.
What is the bigger picture? You say you have decoded some pathways that cause tumor formation. What’s next?
Well, I see it as smoking, except that people with genotoxic microbes involuntarily ‘smoke’ in their gut. So we have a subsidy of 1.3 million. USD from the Ministry of Defense to develop what we call “Colirette”. It is like Nicorette in the sense that we are developing probiotics that you can take to selectively remove genotoxic bacteria from the gut.
Over the next three years, we will develop these probiotics and perform the preclinical work necessary to demonstrate proof of concept for further commercial development.
If you had unlimited resources, what further research would you pursue?
That’s the question we always dream of, not true where someone comes up and gives you a pile of money and you don’t have to write grants anymore.
I’m still very excited about the area of inflammation, and our approaches, I think, are the right approaches. I would systematically expand them if I had unlimited resources because even human metabolism remains a surprisingly undefined area.
If these pathways are associated with regulation of inflammation, then dysregulation of these pathways will naturally be associated with inflammatory disease. There are many inflammatory diseases and we do not do a great deal of work in treating them. We typically treat the symptoms.
But if you figure out these new avenues, you can add the molecules back and restore a level of homeostasis, and I love that these are drugs, except that they are not the traditional drugs that pharma manufactures. They are natural. They already belong in us and we restore a natural process.
We can add the natural connection back instead of an artificial one, which often has off-target effects. Because I’m more into the natural product range, I like the idea of using natural molecules to treat disease.
Researchers identify pathways that are crucial for the development and prevention of intestinal inflammation
Provided by Yale University
Citation: Mining for GEMs: Nature’s Precious Tool for Treating Diseases (2022, January 4) Retrieved January 4, 2022 from https://ift.tt/3qPQHFc .html
This document is subject to copyright. Apart from any reasonable trade for the purpose of private investigation or research, no part may be reproduced without written permission. The content is provided for informational purposes only.
Post a Comment